Your Complete Guide to Diabetic Foot Care: Protecting Your Feet for Life
Most serious diabetic foot complications are preventable. After years of treating patients with diabetes, I’ve seen one thing hold true: the difference between healthy feet and limb-threatening infections often comes down to education and daily habits.
You don’t need a medical degree to protect your feet. You need awareness, a few minutes each day, and the right care team.
Why Feet Need Extra Attention
Your feet are remarkable structures, but they sit at the farthest point from your heart. When you have diabetes, three things often combine to create problems:
High blood sugar damages small blood vessels and weakens the skin and nerves¹.
Neuropathy reduces your ability to feel injuries².
Poor circulation (PAD) narrows arteries and slows healing³.
The result is a “silent storm.” A small blister may go unnoticed, heal poorly, and become infected before you realize something is wrong.
Neuropathy: When Nerves Stop Talking
I’ll never forget a patient who walked in with a severe burn on the bottom of his foot. He had stepped onto hot pavement barefoot but felt nothing because of neuropathy. That’s how sneaky this complication can be.
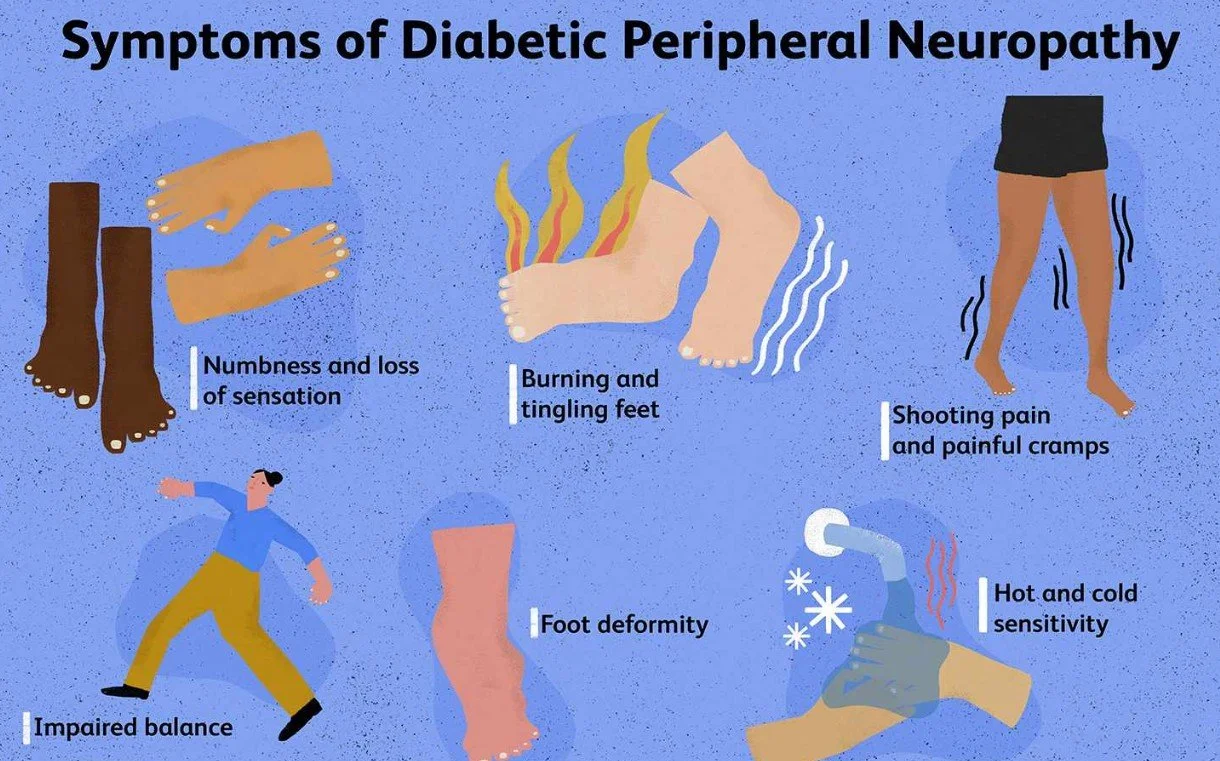
The Three Types of Neuropathy
Sensory neuropathy: Tingling, burning, or numbness; eventually complete loss of protective sensation².
Motor neuropathy: Weak foot muscles cause hammertoes or high arches, creating new pressure points⁴.
Autonomic neuropathy: Sweat glands stop working, leaving skin dry, cracked, and vulnerable⁵.
Why It Matters
Pain is your body’s alarm system. Neuropathy disables that system. A shoe rub, a pebble underfoot, or a small cut may not cause pain but can still escalate into a serious ulcer.
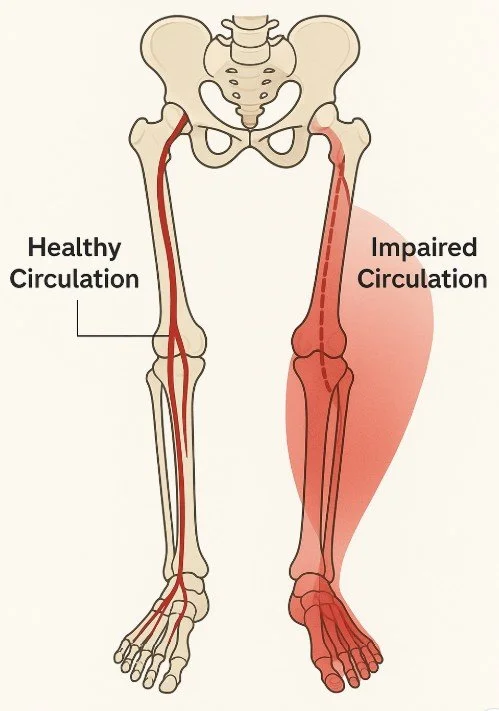
Circulation: Why Blood Flow Matters
When I examine diabetic patients, I always check their pulses at the ankles and feet. I’m looking for peripheral arterial disease (PAD) — a condition that makes healing harder and infections more dangerous.
Common signs include:
Feet that stay cold
Cramping in calves when walking (claudication)
Pale, bluish, or overly red skin
Thin, shiny skin and hair loss on legs
Wounds that heal slowly or not at all³
If you have both neuropathy and PAD, your risk of amputation rises dramatically. Early detection is essential.
The Daily Foot Check: Five Minutes That Matter
This is the most valuable habit you can build. A quick self-exam often detects problems before they become emergencies.
How to do it:
Set up: Find good lighting, sit comfortably, and use a hand mirror or ask a family member to help.
Look for: Cuts, scratches, blisters, swelling, color changes, calluses, or redness around nails.
Check between toes: This area stays moist and is prone to fungus and cracks.
Feel: Run your hands across your feet for lumps, bumps, or tender spots.
Act quickly: Any wound that isn’t improving in 24–48 hours, sudden swelling, or spreading redness needs professional care.
Skin Health: Your First Barrier
Diabetes reduces natural oils and weakens your skin barrier. That’s why dryness, cracks, and slow healing are so common⁵.
Daily routine:
Wash with lukewarm water (never hot).
Dry thoroughly, especially between toes.
Moisturize tops and bottoms with creams that contain urea or lactic acid⁶.
Avoid soaking and avoid chemical corn or callus removers.
These small steps reduce fissures, which are often the doorway for infection.
Nail Health: More Than Cosmetic
Nails can be a hidden problem area. Thick or fungal nails create pressure, trap bacteria, and increase ulcer risk⁷ ⁸ ⁹.
At-home if you’re low risk:
Trim nails straight across.
Use clippers (not scissors).
Smooth edges gently with a file.
See a professional if:
Nails are thick, curved, or discolored.
You have neuropathy or poor circulation.
You’ve had previous nail infections.
Professional trimming prevents many avoidable infections.
Footwear: The Foundation of Prevention
Most diabetic ulcers form under high-pressure spots. The right shoes redistribute that pressure¹⁰.
What to look for:
Extra depth and wide toe box
Seamless, breathable lining
Cushioned midsole, rocker sole, and non-slip outsole
Adjustable closure for swelling
Shopping tips:
Buy shoes in the afternoon when feet are largest.
Bring your socks or inserts.
Make sure there’s a thumb’s width in front of your toes.
Break shoes in slowly.
When to consider prescription shoes: If you have neuropathy, deformities, or a history of ulcers, Medicare often covers therapeutic shoes and inserts¹¹.
When Small Problems Become Big
In diabetes, there is no such thing as a “minor” foot issue.
Red flags that require same-day attention:
Spreading redness, warmth, or swelling
Pus, odor, or fever with a wound
Sudden swollen, red, warm foot (possible Charcot)¹²
New calf pain or a cold pale foot (possible arterial insufficiency)
These changes are emergencies. Do not wait for them to “get better.”
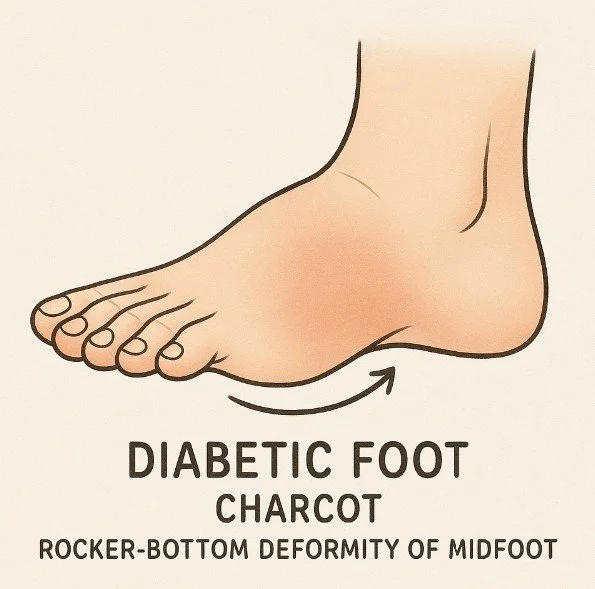
Charcot Foot: The Great Imposter
Charcot neuroarthropathy is one of the most serious but underrecognized diabetic foot complications. It is regularly misdiagnosed with more common conditions like gout, arthritis flares, simple fractures, and infection
What happens: Neuropathy weakens the bones. Small fractures occur without pain. Walking continues, the bones collapse, and the foot deforms¹².
Phases:
Acute: Warm, red, swollen foot (X-rays may be normal).
Coalescence: Inflammation settles, bone begins to heal.
Reconstruction: Bones heal in deformed positions → new pressure points.
Why it matters: If caught in the early phase, immobilization and offloading can prevent collapse.
Building Your Foot Care Plan
Every day:
Inspect both feet and between toes
Wash, dry, moisturize
Wear protective socks and shoes
Keep glucose under control
Every 2-3 months (if high risk):
Professional nail and callus care
Footwear check
Every year (at minimum):
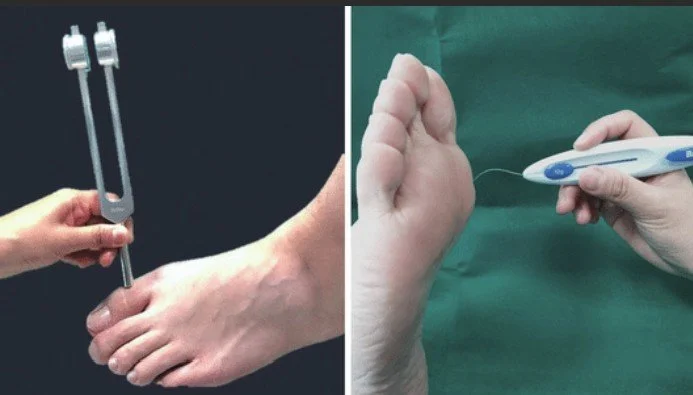
Full podiatry exam
Neuropathy and circulation testing
Shoe/orthotic review¹³
Your care team may include:
Primary care or endocrinologist
Podiatrist
Diabetes educator
Pedorthist/orthotist
Vascular specialist
Quick Red Flag Reference
At least once per year for a comprehensive foot exam. More often if you have neuropathy, circulation problems, or a history of ulcers13.
If your nails are healthy, straight, and you have good vision and sensation, you may trim them straight across. If nails are thick, ingrown, or if you have neuropathy, see a podiatrist8.
Protective footwear reduces risk even in patients without visible deformity. Proper depth, width, and cushioning prevent ulcers before they start10.
Yes. Diabetic skin tends to be dry and prone to cracking. Creams with urea or lactic acid help restore the skin barrier and reduce fissures6.
If you notice spreading redness, swelling, pus, foul odor, or a wound not improving within 48 hours, call the same day. Fever or sudden swelling requires urgent evaluation12.
References
Boulton AJM. The Foot in Diabetes. Wiley, 2020.
Tesfaye S, et al. “Diabetic neuropathies.” Diabetologia. 2020.
Jude EB, et al. “Peripheral arterial disease in diabetic patients.” Diabet Med. 2010.
Menz HB, et al. “Foot problems and falls in older adults with diabetes.” Gerontology. 2013.
American Podiatric Medical Association. Diabetic Foot Care Guidelines.
Parker J, et al. “Moisturisers for foot xerosis.” J Foot Ankle Res. 2017.
Gupta AK, et al. “Onychomycosis in diabetes.” J Eur Acad Dermatol Venereol. 2017.
Armstrong DG, et al. “Ingrown toenails and diabetes.” JFAS. 2002.
Gupta AK, et al. “Fungal nail infections and risk of diabetic foot ulcers.” Diabetes Care. 2016.
Raspovic A, et al. “Footwear interventions to prevent diabetic foot ulcer recurrence.” Diabetes Metab Res Rev. 2016.
CMS. Medicare Coverage for Therapeutic Shoes for Diabetes. 2025.
Rogers LC, et al. “Charcot foot in diabetes.” Diabetes Care. 2011.
American Diabetes Association. Standards of Care in Diabetes, 2025.