Hallux Rigidus (Big Toe Arthritis): What It Is and How to Treat It
If your big toe feels stiff, sore, and hard to bend when you walk, you might be dealing with hallux rigidus — arthritis of the first metatarsophalangeal (MTP) joint. This condition can limit daily walking, sports, and even shoe choice. The encouraging news is that we have both non-surgical and advanced surgical options, including modern minimally invasive techniques that were not widely available even a decade ago.
What Is Hallux Rigidus?
Hallux rigidus is the most common arthritic condition in the foot, affecting about 2.5% of people over age 50¹. The term literally means “stiff toe” in Latin, and refers to degenerative arthritis of the big toe joint. Over time, the smooth cartilage lining the joint wears away, leading to stiffness, pain, and bony overgrowths (spurs). Unlike a bunion, which pushes the toe sideways, hallux rigidus causes the joint to lock up and lose motion.
Research shows that among adults aged 50 and older with foot arthritis (affecting ~17% of this population), approximately 25% have radiographic arthritis of the first MTP joint².
👣 Curious how arthritis differs from bunions? Read our guide on bunions in 2025.
Symptoms to Watch For
Pain and stiffness at the base of the big toe
Pain worse when pushing off (stairs, running, hills)
A bump on top of the joint (dorsal spur)
Limited upward motion (dorsiflexion)
Difficulty with low toe-box shoes
What Causes It?
The cause is often multifactorial. Multiple authors have noted associations with trauma, iatrogenic causes, and family history. Women and those with bilateral involvement are more frequently affected³.
Genetics: Flat or elevated first metatarsal structure (metatarsus primus elevatus) can overload the joint
Injury: Turf toe or repeated trauma can accelerate arthritis
Overuse: Common in athletes and dancers
Inflammatory arthritis: Conditions like rheumatoid arthritis may mimic or worsen the process
Diagnosing Hallux Rigidus
Physical Exam:
Range of motion testing, especially dorsiflexion
Palpation for dorsal osteophytes
Assessment of joint line tenderness
Imaging:
X-rays: Weightbearing AP, lateral, oblique to evaluate joint space, spurs, sesamoid changes
CT: Detailed 3D bone evaluation for surgical planning
MRI: Identifies focal cartilage loss or early arthritis
Coughlin–Shurnas Classification (widely cited, endorsed in ACFAS consensus⁴):
Grade 1: Mild stiffness, minimal radiographic changes
Grade 2: Moderate stiffness, dorsal spurring, joint space narrowing
Grade 3: Severe stiffness, large spurs, marked joint narrowing
Grade 4: End-stage arthritis, near-total motion loss
⚡ Forefoot pain isn’t always arthritis. Learn how sesamoiditis can mimic hallux rigidus.
Treatment Options
Conservative Care
Up to 55% of patients in early stages improve with nonoperative care⁵.
Shoes: Stiff-soled, rocker-bottom shoes (Hoka Bondi, Brooks Ghost Max) reduce painful motion
Orthotics:
Custom foot orthoses to offload the joint
Carbon fiber Morton’s extension — a rigid plate under the big toe that blocks painful dorsiflexion while still fitting into normal shoes
Other measures:
Activity modification (limiting barefoot/high-impact activity during flares)
Short courses of NSAIDs
Corticosteroid injections (variable relief, not long-term)
Surgical Options
Choice depends on severity, activity goals, and arthritis grade.
1. Cheilectomy (Spur Removal and Joint Cleanup)
Removes dorsal spurs and smooths cartilage
Best for mild to moderate arthritis
Preserves motion and allows sports return
Modern option:
Minimally Invasive Cheilectomy (Stryker system): 3–5 mm portals, fluoroscopic guidance, high-speed burr. Benefits include reduced soft tissue disruption, smaller scars, faster swelling resolution (average 5 weeks), and high satisfaction rates⁶.
2. Osteotomy
Bone cut to realign or shorten metatarsal
Indicated in patients with structural overload
Often paired with cheilectomy
3. Cartilage Procedures
Microfracture or cartilage grafting for focal lesions
Limited long-term evidence in the first MTP joint
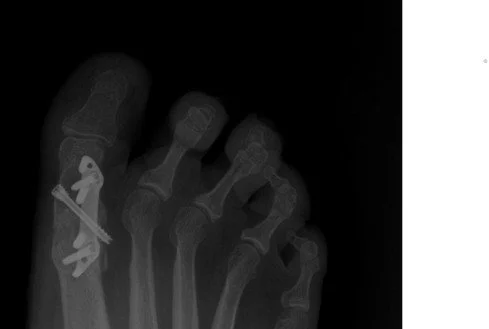
4. Arthrodesis (Fusion)
Gold standard for advanced arthritis (AOFAS/ACFAS consensus)
95% union rates, durable pain relief beyond 10 years⁷
Eliminates painful motion but preserves functional gait
Modern options:
MIS Fusion (Stryker platform): Keyhole access, less dissection, fluoroscopic control
Treace First MTP Fusion System: Low-profile contoured plate with crossing screws, designed for anatomic alignment and earlier weightbearing
5. Arthroplasty (Joint Replacement/Interpositional)
Motion-preserving alternative
Silicone/metallic implants = variable long-term survival
Interpositional arthroplasty (biologic spacers) for select patients
Less common today due to reliability of fusion
| Procedure | Best For | Pros | Cons | Recovery |
|---|---|---|---|---|
| Cheilectomy (Open or MIS) | Mild–moderate arthritis | Preserves motion; MIS = smaller scar, less swelling | May fail in advanced disease | Return in 6–8 weeks |
| Osteotomy | Structural overload cases | Corrects mechanics; may delay arthritis | Technically demanding; limited indications | Boot 4–6 weeks |
| Fusion (Arthrodesis) | Severe arthritis | Gold standard; >95% union; Treace = early weightbearing | Loss of motion; no high heels | Boot 6–8 weeks |
| Arthroplasty | Select motion-seeking patients | Preserves motion | Higher revision rates; less predictable | Variable |
Recovery Timelines
MIS Cheilectomy: Walking within days, activity 6–8 weeks
Open Cheilectomy: Similar timeline, more swelling/bruising
MIS or Treace Fusion: Protected WB ~6 weeks, excellent durability
Replacement: Similar early recovery, but higher revision risk
Prevention and Long-Term Outlook
Choose stiff-soled shoes and wide toe boxes early
Address injuries promptly
Do not ignore swelling or early spurs
Early intervention = more surgical options beyond fusion
With proper care — conservative or surgical — most patients return to daily activity with significant pain reduction and functional improvement.
❓ Frequently Asked Questions
Is hallux rigidus the same as a bunion?
No. A bunion drifts sideways, while hallux rigidus causes stiff, arthritic loss of motion.
Can I still run after fusion?
Yes. Most patients run, hike, and cycle pain-free after fusion, though high-heel use is limited.
Is MIS fusion as durable as open fusion?
Early results are promising, but ACFAS still considers open fusion the benchmark until more long-term data exists.
Do all cases need surgery?
No. Many patients do well for years with shoe changes, orthotics, and Morton’s extensions.
👣 Feet Made Simple Resource Box
- Brooks Ghost Max 3 – rocker sole shoe for forefoot arthritis relief
- Hoka Bondi 9 – cushioned stiff-soled shoe to reduce big toe stress
- Topo Ultraventure 4 – wide toe box for bunion and hallux rigidus comfort
- Carbon Fiber Morton’s Extension – limits painful big toe motion while walking
References
Coughlin MJ, Shurnas PS. Hallux rigidus: demographics, etiology, and radiographic assessment. Foot Ankle Int. 2003;24(10):731-743.
Roddy E, Thomas MJ, Marshall M, et al. The population prevalence of symptomatic radiographic foot osteoarthritis. Arthritis Care Res. 2015;67(9):1312-1319.
ACFAS Clinical Consensus Statement: Diagnosis and treatment of first MTP disorders. J Foot Ankle Surg. 2015;54(6):103-115.
Easley ME, Trnka HJ. Current concepts review: hallux rigidus. J Bone Joint Surg Am. 2007;89(5):991-1002.
Grady JF, Axe TM, Zager EJ, Sheldon LA. A retrospective analysis of 772 patients with hallux rigidus. J Am Podiatr Med Assoc. 2002;92(2):102-108.
Waizy H, et al. Minimally invasive cheilectomy for hallux rigidus: short-term outcomes. Foot Ankle Surg. 2017;23(2):122-126.
Bussewitz BW, Hyer CF. Early weightbearing following first MTP fusion using locking plate fixation. Foot Ankle Spec. 2015;8(1):28-33.
Roukis TS. Outcomes of metallic hemiarthroplasty for hallux rigidus. J Foot Ankle Surg. 2011;50(6):707-713.