Achilles Tendinopathy: Your Complete Guide to Understanding and Healing
If you wake up in the morning and feel a tight, sore pull at the back of your heel that gradually loosens as you move, your Achilles tendon may be the culprit. This rope-like structure is the strongest tendon in your body, yet when it breaks down it reminds you with every step.
The good news? Most people improve without surgery if they follow a structured plan. Let’s walk through what works and what doesn’t based on research and thousands of patients I’ve treated.
What Exactly Is Achilles Tendinopathy?
The Achilles tendon connects your calf muscles (gastrocnemius and soleus) to your heel bone (calcaneus). It’s built to handle forces up to 12 times your body weight when running and jumping.¹
When healthy, its fibers line up in neat bundles like strands of a rope. In tendinopathy, those fibers lose alignment, swell, and weaken. Instead of a normal healing response, the tendon gets “stuck” in a degenerative cycle. This is not just inflammation, it’s a failed repair process.¹³
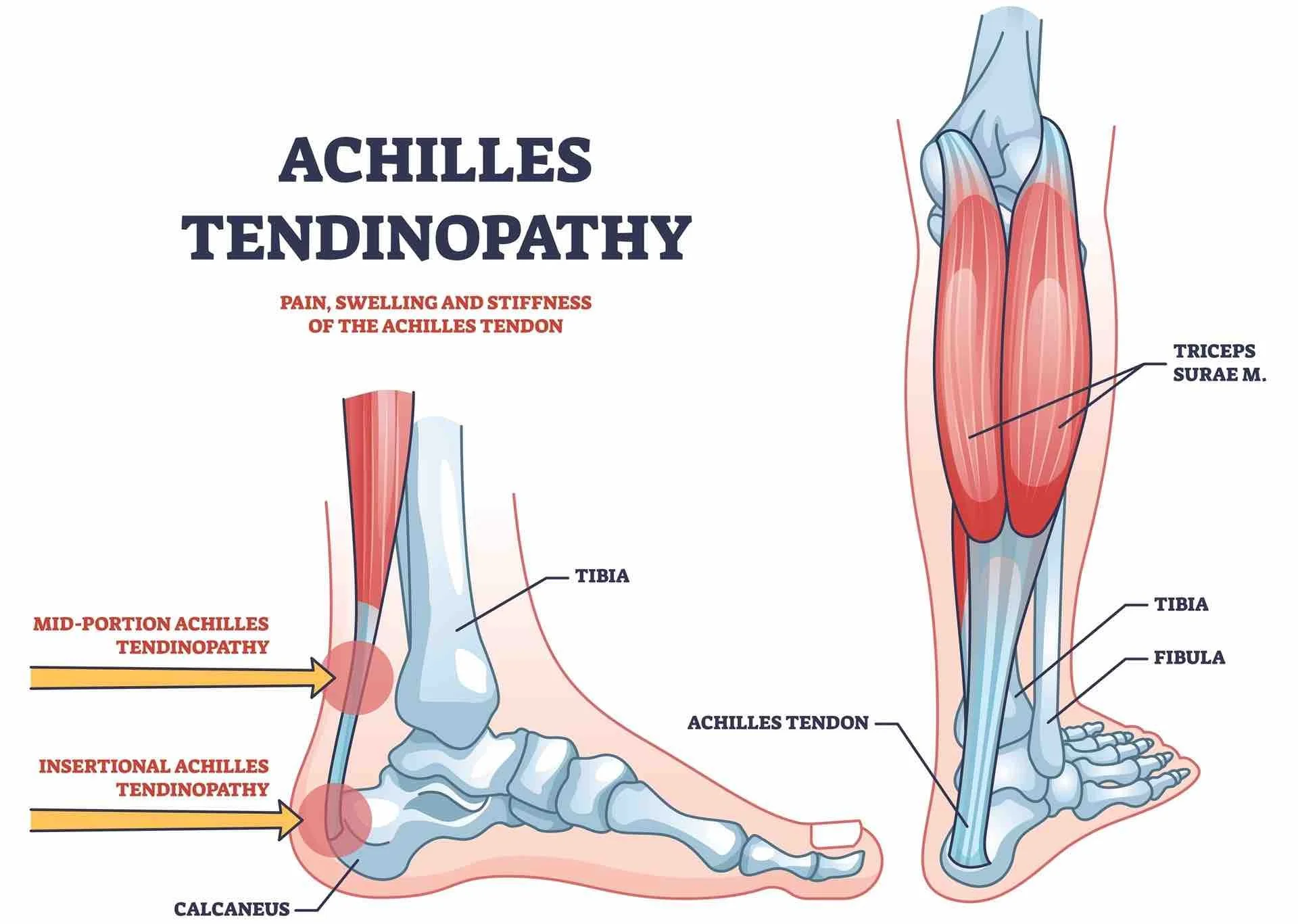
Two Main Types
Midportion tendinopathy: Pain and thickening 2–6 cm above the heel bone. Common in runners and jumpers.
Insertional tendinopathy: Pain right at the heel bone attachment, often aggravated by shoes pressing on the back of the heel, uphill running, or deep ankle bending.³
Not all heel pain is the Achilles: Compare with classic plantar fasciitis. Forefoot overload can flare up when trying to lift up your heel for relief sesamoiditis.
Why Did This Happen to Me?
The Achilles is powerful but vulnerable due the stress across it and the relative lack of blood flow to heal that stress
. Common causes include:
Training errors: mileage or intensity jumps, quick return after significant time not training, excessive hill work²
Tight calves: limited ankle dorsiflexion increases tendon strain³
Footwear issues: worn-out shoes or overly soft soles altering mechanics⁴
Systemic risks: diabetes, obesity, corticosteroids, fluoroquinolone antibiotics (Ciprofloxacin/Levofloxacin)³
Age-related change: less elastic collagen makes tendons less resilient
Think of a rope that’s been weathered and dried — strain it too quickly and fibers fray.
What Does It Feel Like?
Typical symptoms include:
Morning stiffness in the back of the heel or tendon that eases with movement
Tenderness in a specific spot when pressed
Pain with push-off, running, or climbing stairs
Pain after rest (especially sit-to-stand after inactivity)
Thickened or swollen tendon that may look or feel enlarged
Occasional sharp, burning, or pinching pain at the back of the heel
This is different from plantar fasciitis, which causes pain under the heel.
How We Diagnose It
In the clinic
Pinpointing tenderness and thickening
Testing calf flexibility and ankle range of motion
Single-leg heel raises to assess tendon strength
Watching gait mechanics
Imaging
Ultrasound: tendon thickness, fiber disorganization, abnormal blood vessels
MRI: complex or surgical planning cases, suspected tears
X-ray: insertional cases with bone spurs or Haglund’s deformity³
| Feature | Midportion | Insertional |
|---|---|---|
| Pain location | 2–6 cm above the heel bone | At the tendon attachment to the heel |
| Common triggers | Running or jumping and sudden training spikes | Shoes pressing on the back of the heel and uphill running |
| First line rehab | Step eccentrics with slow control | Flat ground eccentrics and temporary heel lifts |
| Adjuncts | Physical therapy and dry needling and isometrics as needed | Physical therapy and heel lifts with careful load progression |
| Surgery options | Debridement and gastrocnemius recession in select cases | Debridement and calcaneoplasty and Zadek calcaneal osteotomy |
Treatment: What Actually Works
1. Load Management
Healing requires activity, but the right kind and amount. Morning stiffness and pain are your guide. If it worsens after activity, you did too much. If it’s stable or better, you’re on target.¹
2. Exercise Therapy (The Foundation)²⁴
Midportion: Heel drops off a step or similar ledge, controlled eccentrics
Insertional: Start flat or with a heel lift, then gradually increase range
Timeline: At least 12 weeks of progressive training (tendons heal slower than muscles)
3. Physical Therapy
Working with a PT makes a real difference. Programs usually include:
Heavy slow resistance or eccentric loading adjusted to tolerance²⁴
Isometric calf holds for early pain relief²
Manual therapy and mobility drills to improve ankle flexibility
Movement retraining to address running and gait mechanics
Supervised PT improves adherence and outcomes more than “just doing exercises at home.”³⁵
4. Dry Needling
Dry needling uses thin needles inserted into the tendon or nearby muscles to stimulate healing.
An RCT showed dry needling + eccentric exercise improved VISA-A scores more than exercise alone.⁶
It likely works by disrupting degenerative tissue, triggering localized repair, and reducing pain sensitivity.⁷
Best used alongside PT — not as a stand-alone treatment.
Achilles Dry Needling with electrical stimulation
a highly effective option especially for chronic or resistant cases
5. Footwear & Orthotics
Cushioned, rockered trainers decrease tendon load
Supportive midsoles and roomy toe boxes improve mechanics
Temporary 6–8 mm heel lifts help insertional pain
Affiliate placeholders: Brooks Ghost Max, Hoka Bondi, Topo Magnifly, heel lifts
6. Stretching & Night Splints
Gentle calf stretching (knee straight and bent) once pain calms. Adjustable Night splints can reduce severe morning stiffness.³
7. Injections?
PRP hasn’t consistently shown better results than exercise programs. I discuss it openly but temper expectations.⁸
Pediatric Corner: Heel Pain in Kids
In children, true Achilles tendinopathy is rare. Most heel pain is calcaneal apophysitis (Sever’s disease) — irritation of the growth plate.
Treatment is refreshingly simple:
Activity as tolerated
Cushioned shoes or heel cups
Ice after play
Calf stretching
Kids nearly always outgrow it as the growth plate closes.⁷
Parent tip: If your child’s limp eases after rest and a heel cup, you’re on the right track.
Sports Medicine Considerations
Load progression must fit the sport (running vs jumping vs cutting)
Early imaging is justified for suspected rupture or high-grade tear
PT & dry needling are strong adjuncts to keep athletes training while rehabbing⁶⁷
Return-to-play after surgery: often 4–6 months, guided by strength, hop tests, and plyometric readiness¹¹
When Conservative Care Isn’t Enough
Surgery is considered only after 6+ months of structured care without progress.
Midportion Options
Debridement of degenerative tissue and usually reinforce with native or synthetic tissue. I have been really liking a graft called Artelon the past year doing a box weave reinforcement technique.
Gastrocnemius recession when calf tightness drives persistent symptoms⁹
Insertional Options
Debridement + bursectomy
Calcaneoplasty for bony impingement
Zadek Calcaneal Osteotomy: a dorsal wedge osteotomy that repositions the calcaneus, reduces compression, and preserves the tendon. Minimally invasive approaches show excellent results with quicker recovery.¹²¹³
My approach: I frequently use the minimally invasive Zadek osteotomy for stubborn insertional cases. It preserves tendon attachment and aligns well with modern tendon-sparing principles.
More foot overload mechanics: Nerve‑type forefoot pain points toward Morton’s neuroma. If your big toe crowds in shoes, review modern options for bunions.
Recovery Timeline
Weeks 0–2: Relative rest, cycling or swimming, isometric holds
Weeks 2–6: Begin eccentrics, progress seated → standing → single-leg heel raises
Weeks 6–12: Increase load, add hopping and plyometrics once pain-free
Return to sport: gradual, guided by PT and pain-free testing²
Prevention Tips
Increase activity gradually (≤10% per week)
Replace worn-out shoes before midsoles collapse
Maintain calf strength and flexibility all year
Don’t push through worsening morning stiffness — it’s an early warning sign
Bottom Line
Achilles tendinopathy is frustrating, but with the right plan most people recover fully. Structured exercise and PT remain the foundation. Dry needling offers another tool for stubborn cases. Kids usually bounce back quickly from growth plate irritation, and athletes can return to full performance with patient load progression.
For the small group who fail conservative care, tendon-preserving surgical options like the minimally invasive Zadek osteotomy give excellent outcomes.
The key is starting early, staying consistent, and respecting your tendon’s timeline.
Achilles Tendinopathy FAQ
Is Achilles tendinopathy the same as a tear?
No. Tendinopathy is a load tolerance problem in the tendon. A full tear is an acute rupture. Exam and history separate them.¹
Do I rest completely or keep moving?
You keep moving within pain‑guided limits. The tendon needs progressive loading to remodel and regain strength.¹
Does dry needling or physical therapy help?
Yes when combined with a structured loading program, calf mobility, and shoe support. Consistency matters more than any single modality.¹
¹ References align with the main article’s citations from peer‑reviewed sources including JFAS, APMA, and AOFAS.
🦶 Recommended Products for Achilles Tendinopathy
These items are listed for education and reference only. They are not a substitute for medical advice. Please see your podiatrist for specific recommendations. I may receive a commission if you purchase through these links, at no additional cost to you.
👟 Shoes
- Hoka Bondi 9 – Plush maximalist shoe to reduce Achilles strain
- Hoka Skyline Float-X – Stable rocker sole option for activity
- Brooks Ghost Max 3 – Rocker bottom design to ease calf tension
🩴 Sandals
- OOfos Recovery Sandal – Reduces load post-exercise or after long days
🧰 Rehab Tools
- Wedge Stretch Device – Helps stretch the calf and Achilles safely
- Rigid Night Splint – Maintains calf stretch overnight
- Theraband Resistance Bands – For eccentric calf strengthening
References
¹ Cook JL, Purdam CR. Revisiting the continuum model of tendon pathology. Br J Sports Med. 2016.
² Alfredson H, Pietilä T, Jonsson P, Lorentzon R. Heavy load eccentric calf training for chronic Achilles tendinosis. Am J Sports Med. 1998.
³ Chimenti RL, et al. Insertional Achilles tendinopathy: Current concepts. Int J Sports Phys Ther. 2017.
⁴ Jayaseelan DJ, et al. Eccentric exercise for Achilles tendinopathy: A systematic review. Int J Sports Phys Ther. 2019.
⁵ Murphy M, Travers M, Gibson W. The role of supervised rehabilitation in Achilles tendinopathy: Systematic review. Phys Ther Sport. 2019.
⁶ Krey D, Borchers J, McCamey K. Efficacy of dry needling in tendinopathy: A randomized controlled trial. Clin J Sport Med. 2017.
⁷ Navarro-Santana MJ, et al. Effects of dry needling on tendinopathy: Systematic review and meta-analysis. Pain Med. 2020.
⁸ de Vos RJ, et al. Platelet-rich plasma injection for chronic Achilles tendinopathy. JAMA. 2010.
⁹ Kiewiet NJ, et al. Gastrocnemius recession for chronic noninsertional Achilles tendinopathy. Foot Ankle Int. 2013.
¹¹ Lee KT, et al. Return to play after open calcaneoplasty. Orthop J Sports Med. 2021.
¹² Poutoglidou F, et al. Zadek calcaneal osteotomy in insertional Achilles tendinopathy: Systematic review. Foot Ankle Surg. 2023.
¹³ Kaplan JRM, Vulcano E. Percutaneous Zadek osteotomy for insertional Achilles tendinopathy. Foot Ankle Int. 2023.