Ankle Sprains: Your Complete Recovery and Prevention Guide
Rolling your ankle can turn a good day upside down in an instant. The good news? Most ankle sprains heal with the right approach. Here’s everything you need to know to recover fully and prevent the next one, backed by the latest research from the American Orthopaedic Foot & Ankle Society (AOFAS), the Journal of Foot & Ankle Surgery (JFAS), and other leading organizations.
What Actually Happened to Your Ankle
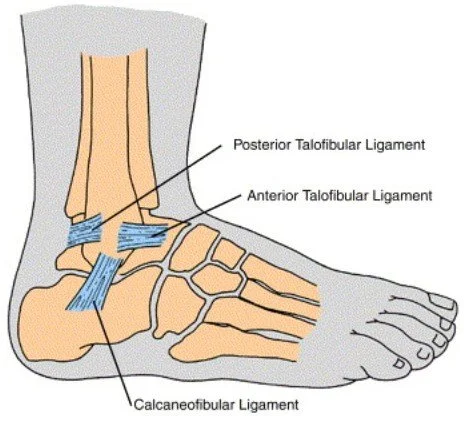
When you “roll” your ankle inward, you’re stretching or tearing the ligaments on the outside of your ankle, usually the anterior talofibular ligament (ATFL) and the calcaneofibular ligament (CFL). Think of these as small, strong cables that keep your ankle stable when you walk, run, or change direction.
The injury can range from a mild stretch (Grade 1), to a partial tear (Grade 2), to a complete rupture (Grade 3). The important thing to know is that it takes four to five days for swelling to settle before we can accurately grade the severity. This is why many foot and ankle surgeons, including myself, recommend a follow-up visit rather than making every decision on the first day.¹
Do You Need X-rays?
Not every ankle sprain requires an X-ray. To avoid unnecessary radiation and cost, we often use the Ottawa Ankle Rules in clinic, a set of validated guidelines developed in Ottawa, Canada, to determine when imaging is necessary.² ³
You should have X-rays if you have:
Ankle pain plus bone tenderness at either the inner or outer ankle bone (medial or lateral malleolus)
Inability to take four steps immediately after the injury
These rules are highly sensitive for fractures that need urgent care and have been validated in both adult and pediatric populations.
👉 Struggling with calf tightness or tendon pain? Learn more in our Achilles Tendinopathy Guide.
Your Recovery Roadmap: PEACE & LOVE
The American Physical Therapy Association (APTA) updated its 2021 Clinical Practice Guidelines to recommend the PEACE and LOVE model for acute musculoskeletal injuries.⁴ This approach moves beyond the old “RICE” (rest, ice, compression, elevation) method and reflects modern evidence.
First 72 Hours: PEACE Protocol
Protect: Use crutches, a supportive brace, or boot as needed
Elevate: Prop the ankle above heart level whenever possible
Avoid anti-inflammatories initially: NSAIDs may slow early ligament healing
Compress: Use wraps or semi-rigid braces to control swelling
Educate: Understand what to expect in your recovery
After 72 Hours: LOVE Protocol
Load: Begin gentle weight-bearing as pain allows
Optimism: Research shows mindset influences healing outcomes
Vascularization: Use light cardio like cycling or pool walking to pump blood flow
Exercise: Restore mobility, balance, and strength
Week-by-Week Recovery Plan
Evidence from AOFAS protocols and systematic reviews helps outline a timeline for most patients.⁵
Week 0–1: Protection Phase
Wear a lace-up ankle brace or short walking boot for comfort
Gentle ankle circles and “alphabet writing” to maintain motion
Early walking within pain limits is encouraged—strict immobilization delays healing
Keep swelling down with compression and elevation
Weeks 1–3: Motion and Balance
Focus on regaining ankle flexibility, especially dorsiflexion (bending the foot upward)
Start balance drills: stand on one foot, then progress to wobble boards or foam pads
Add low-impact cardio like stationary biking or pool walking
Manual therapy from a physical therapist can help restore mobility
Weeks 3–6: Strength and Function
Add resistance band strengthening for the ankle muscles
Begin sport-specific drills while wearing ankle support
Progress to hopping, cutting, and pivoting as tolerated
Continue neuromuscular training—critical for preventing repeat injuries
Pediatric Pearls: Ankle Sprains in Kids
Children don’t always injure their ankles like adults. Because their growth plates are still open, injuries can mimic a sprain but actually involve the bone. In the past, these injuries were automatically treated with a cast. Today, research published in the Journal of Foot & Ankle Surgery (JFAS) shows that many children with normal X-rays recover just as well with:⁶
A removable ankle brace instead of a cast
Modified activity rather than strict rest
Simple, home-based rehabilitation exercises
Red flags for parents:
Severe limp or refusal to walk
Bone tenderness near the growth plate
No improvement after one week
Prevention for young athletes:
Balance training (20–30 minutes, three times a week for 4–6 weeks) reduces reinjury risk by up to 50%⁷
Proper footwear—cleats or court shoes that resist rolling
Structured return-to-play instead of relying only on “it feels fine today”
👉 Parents: curious about arch development? Read our Pediatric Flatfoot Guide.
Returning to Sports Safely: The PAASS Framework
Athletes and weekend warriors often ask me, “When can I get back in the game?” The answer is not about a calendar date—it’s about function. Sports medicine specialists recommend the PAASS framework, which stands for:⁸
Pain: Minimal during activity
Ankle impairments: Strength and mobility restored
Athlete perception: Confidence in the ankle
Sensorimotor control: Normal balance and coordination
Sport performance: Skills at pre-injury level
👉 If morning heel pain slows your comeback, check out our Plantar Fasciitis Guide.
When Sprains Become Chronic
If your ankle keeps “giving way” months after the initial injury, you may have chronic ankle instability. This condition develops when the ligaments don’t fully heal and the ankle’s position sensors (proprioceptors) fail to reset. Research in JFAS shows chronic instability increases the risk of cartilage damage and early arthritis.⁹
Non-Surgical Treatment
Comprehensive physical therapy focused on strength, balance, and neuromuscular control
Progressive drills moving from stable surfaces to dynamic challenges
Semi-rigid bracing during high-risk activities—shown to reduce recurrence rates significantly
Surgical Options
Most people, adults and teens alike, recover without surgery. But if you still have instability after 3–6 months of quality rehab, surgical repair may be the best option.
Modified Broström Repair: The gold standard procedure that tightens and reattaches the ATFL and CFL with small anchors. Excellent outcomes and decades of use.¹⁰
Internal Brace Augmentation: A modern technique where high-strength suture tape reinforces the repair, like a seatbelt. Studies in JFAS show patients often return to sport faster and maintain excellent outcomes at 5 years.¹¹
Synthetic Ligament Options (Artelon): Artelon is a synthetic polymer scaffold used in complex or revision cases. It provides additional support while natural tissue heals. Early research suggests it is safe and durable, though best practices are still evolving.¹²
👉 Inside ankle pain that doesn’t feel like a sprain may be Posterior Tibial Tendon Dysfunction (Adult Flatfoot).
Prevention Strategies That Actually Work
A 2022 systematic review (using PRISMA guidelines) summarized six best practices for both treatment and prevention:¹³
Immediate Care
Ottawa Ankle Rules for imaging decisions
Cryotherapy for pain and swelling
Functional supports (braces, tape) over rigid immobilization
Early ambulation when tolerated
Short course of NSAIDs if pain requires it (preferably after 72 hours)
Manual therapy techniques from a physical therapist
Long-Term Prevention
Balance training: 20–30 min, three times a week for 4–6 weeks cuts reinjury risk nearly in half⁷
Game-day bracing: Semi-rigid braces for the first 3 months back reduce risk without limiting performance¹⁴
Strength maintenance: Keep calf and peroneal muscles strong with ongoing exercise
Recovery Timeline (What to Expect)
Grade 1 (Mild): Walking in 1–3 days; sport drills in 2–3 weeks
Grade 2 (Moderate): Bracing for 3–6 weeks; return to cutting/pivoting by 4–6 weeks
Grade 3 (Severe): Rehab for 6–12 weeks; surgical evaluation if instability persists
When to Call Your Podiatrist
Schedule a follow-up if you notice:
No improvement after 4–6 weeks
Deep joint pain, catching, or locking
Persistent swelling or stiffness
Repeated giving way episodes
Sometimes advanced imaging (MRI or ultrasound) is needed to check for cartilage injuries or tendon tears that often accompany ankle sprains.
🦶 Products I Recommend for Ankle Sprains
These products support each stage of ankle sprain recovery—from early protection, through rehab, to safe return to sport. They are curated from my clinical experience and research-backed recommendations.
🩹 Early Protection
- ASO Lace-Up Ankle Brace – Semi-rigid support that stabilizes the ankle during the first weeks.
- Cold Therapy Ankle Ice Pack – Wraparound ice pack to reduce swelling and pain early on.
💪 Rehab & Strength
- Theraband Resistance Bands – For ankle strengthening and restoring stability.
- Wobble Board – Proprioception training tool proven to cut reinjury risk nearly in half.
🏃 Return to Sport & Prevention
- Brooks Ghost Max 3 – Rocker sole running shoe to support a smooth stride during return to play.
- Altra Torin 8 – Zero-drop cushioned shoe promoting natural foot mechanics.
- Compression Ankle Brace – Light support for swelling and added confidence during activity.
- Cleat-Specific Ankle Brace – Slim brace designed to fit inside athletic shoes and cleats.
Note: These are general recommendations I use in practice. Some links are affiliate links which support Feet Made Simple at no cost to you. Always confirm with your provider before starting new treatments.
References
Delahunt E, et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations. British Journal of Sports Medicine. 2018.
Bachmann LM, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot: systematic review. BMJ. 2003.
Dowling S, et al. Accuracy of Ottawa ankle rules to exclude fractures of the ankle and mid-foot in children: a prospective study. Academic Emergency Medicine. 2009.
Martin RL, et al. Ankle Stability and Movement Coordination Impairments: Lateral Ankle Ligament Sprains Revision 2021 Clinical Practice Guidelines. Journal of Orthopaedic & Sports Physical Therapy. 2021.
Polzer H, et al. Treatment of acute ankle injuries: a systematic review. Archives of Orthopaedic and Trauma Surgery. 2022.
Clark KD, et al. Management of acute ankle sprains in pediatric patients: current concepts. Journal of Foot & Ankle Surgery. 2020.
Zech A, et al. Neuromuscular training for rehabilitation and prevention of sports injuries: a systematic review with meta-analysis. Medicine & Science in Sports & Exercise. 2009.
Hertel J. Return to play following lateral ankle sprain: incorporating the PAASS framework. International Journal of Sports Physical Therapy. 2019.
Gribble PA, et al. Evidence review for the 2016 International Ankle Consortium consensus statement on the prevalence, impact and long-term consequences of lateral ankle sprains. British Journal of Sports Medicine. 2016.
Gould N, et al. Early and late repair of lateral ligament of the ankle. Foot & Ankle. 1980.
Cho BK, et al. Outcomes of the modified Broström procedure augmented with suture-tape for ankle instability in patients with generalized ligamentous laxity. Foot & Ankle International. 2019.
Caprio A, et al. Functional outcomes of Artelon ligament augmentation for chronic lateral ankle instability: a prospective study. Journal of Foot & Ankle Surgery. 2018.
Vuurberg G, et al. Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline. British Journal of Sports Medicine. 2018.
Olmsted LC, et al. Efficacy of the Star Excursion Balance Test in detecting reach deficits in subjects with chronic ankle instability. Journal of Athletic Training. 2002.